Subdural hemorrhage (bleeding on the brain)
From trauma or leaky blood vessels?
One of the conundrums of the shaken baby hypothesis has been if the cortical bridging veins were sheared off from shaking as hypothesized, why was there so little blood in these thin film subdural hemorrhages? The brain swelling response in these infants seems disproportionate to the relatively minor amount of subdural hemorrhage, if one assumes the small subdural hemorrhages are caused by trauma.
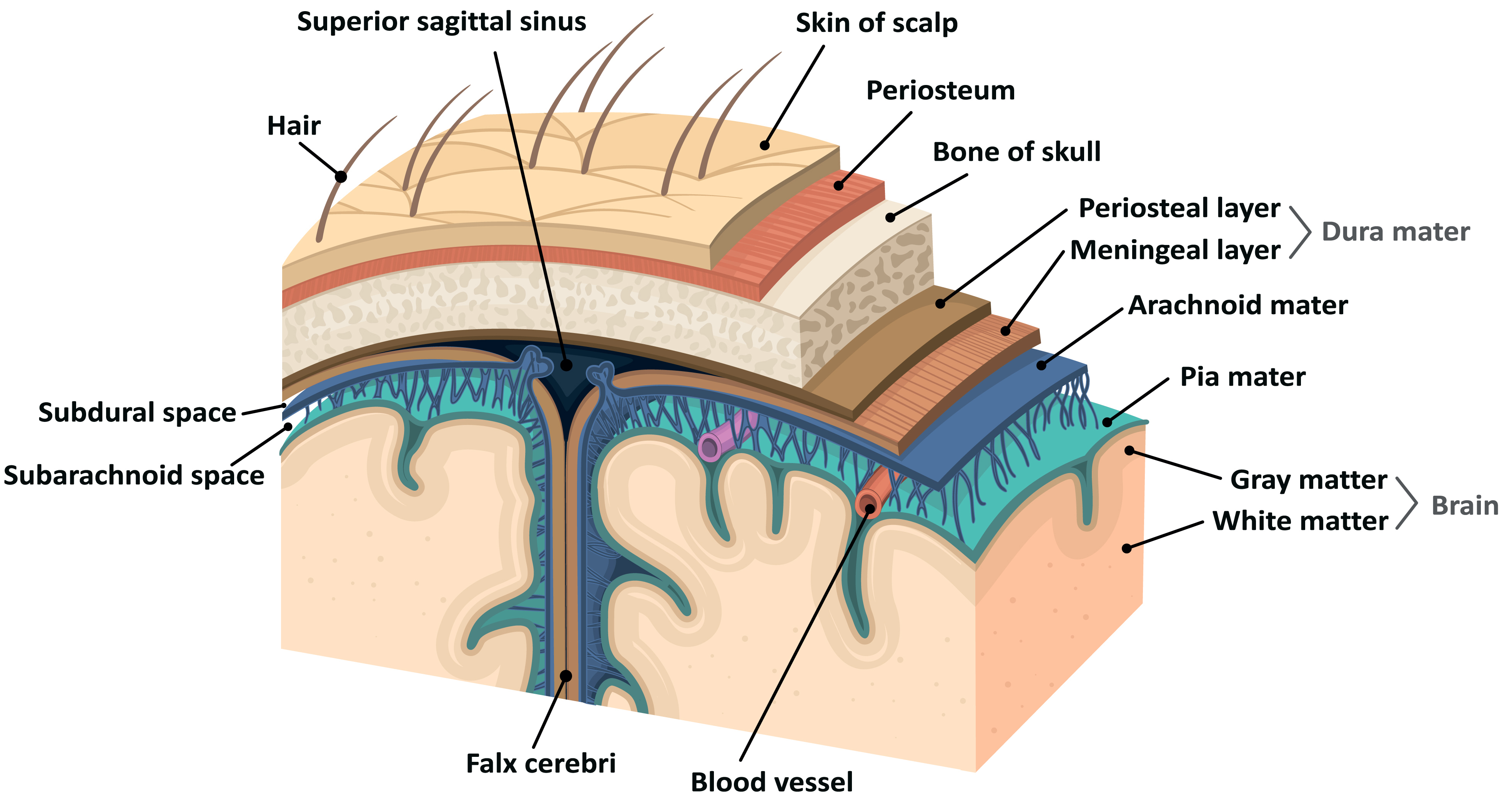
Fig. 1: Layers of the skull & brain
In 2007, a prominent proponent of the shaking hypothesis recognized the conundrum “occurs uniquely in infants and toddlers [and] more likely reflects their age-dependent brain response to combined stresses rather than reflecting a single, specific mechanism or circumstance of injury.”[12] In 2009, a groundbreaking article rediscovered the anatomy of the dura, anatomy that had been forgotten with the advent of CT and MRI imaging technology[13]. A rich vascular network that supplies and drains blood from the dura, and leaks blood under certain natural non-traumatic circumstances, is the likely source of much of the “subdural” bleeding that proponents of shaking presumptively attributed to trauma. The source of the thin film subdural hemorrhage was better explained by leaky blood vessels, rather than by the presumption of trauma.
Brain injury and shearing diffuse axonal injury
From trauma or not enough oxygen?
Shaking, it was hypothesized, sheared brain axons in a pattern distributed diffusely throughout the brain rather than in one particular location, as would be expected in impact trauma. According to the hypothesis, shaking caused diffuse axonal injury (DAI) thus accounting for shaken baby syndrome symptoms of “an immediate decrease in the level of consciousness (either lethargy or unconsciousness); respiratory irregularity, difficulty, or apnea; and frequently seizures”[14] sometimes leading to death. Thus, according to the hypothesis, the caregiver present with the child at the onset of symptoms became the presumptive perpetrator. In 2001 a pair of seminal papers announced findings made possible by new pathological techniques that, in autopsies of cases of hypothesized shaking, the brain did not show torn axons or diffuse axonal injury[15]. By 2010, even one of the foremost shaking advocates conceded that, “[i]t is becoming increasingly clear from both neuroimaging studies and post-mortem analyses of fatal cases that the widespread cerebral and axonal damage in cases of [shaking] are, in fact, ischemic [from inadequate blood flow] rather than directly traumatic in nature.”[16]
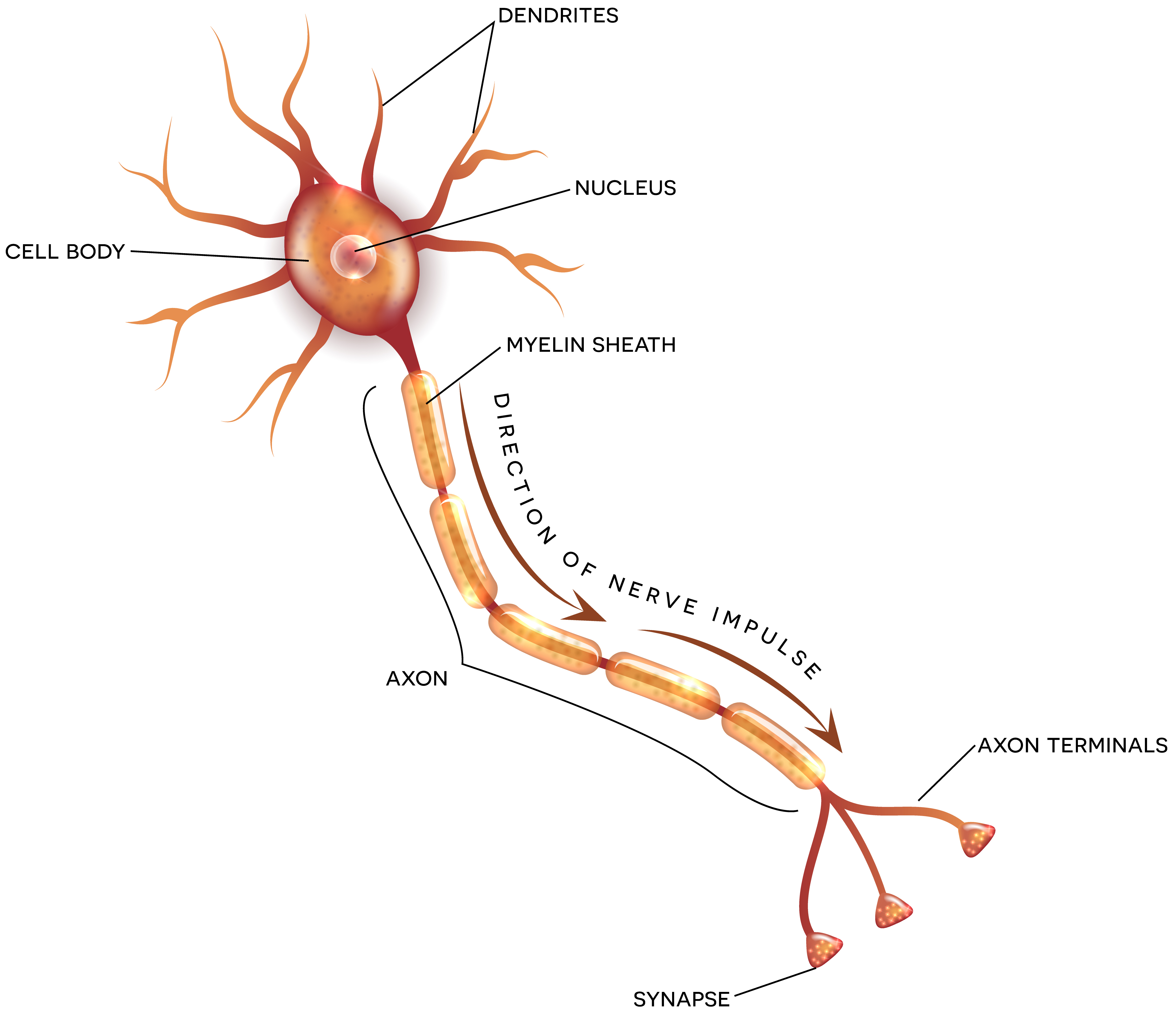
Fig. 2: Anatomy of a neuron
Retinal hemorrhage and retinoschisis
From cardinal and pathognomonic to controversy and doubt
Proponents of the hypothesis increasingly came to rely on the retinal hemorrhage leg of the triad as evidence surfaced that the other two triad legs were not supported by science or medicine. Proponents of the shaking hypothesis assert that “[r]etinal hemorrhages are a cardinal manifestation of abusive head injury characterized by repeated acceleration–deceleration with or without blunt impact (Shaken Baby syndrome).[17] In 2000, one leading shaking proponent boldly declared, macular[18] “retinoschisis has never been described in children due to any entity other than SBS so its presence is diagnostic.”[19]
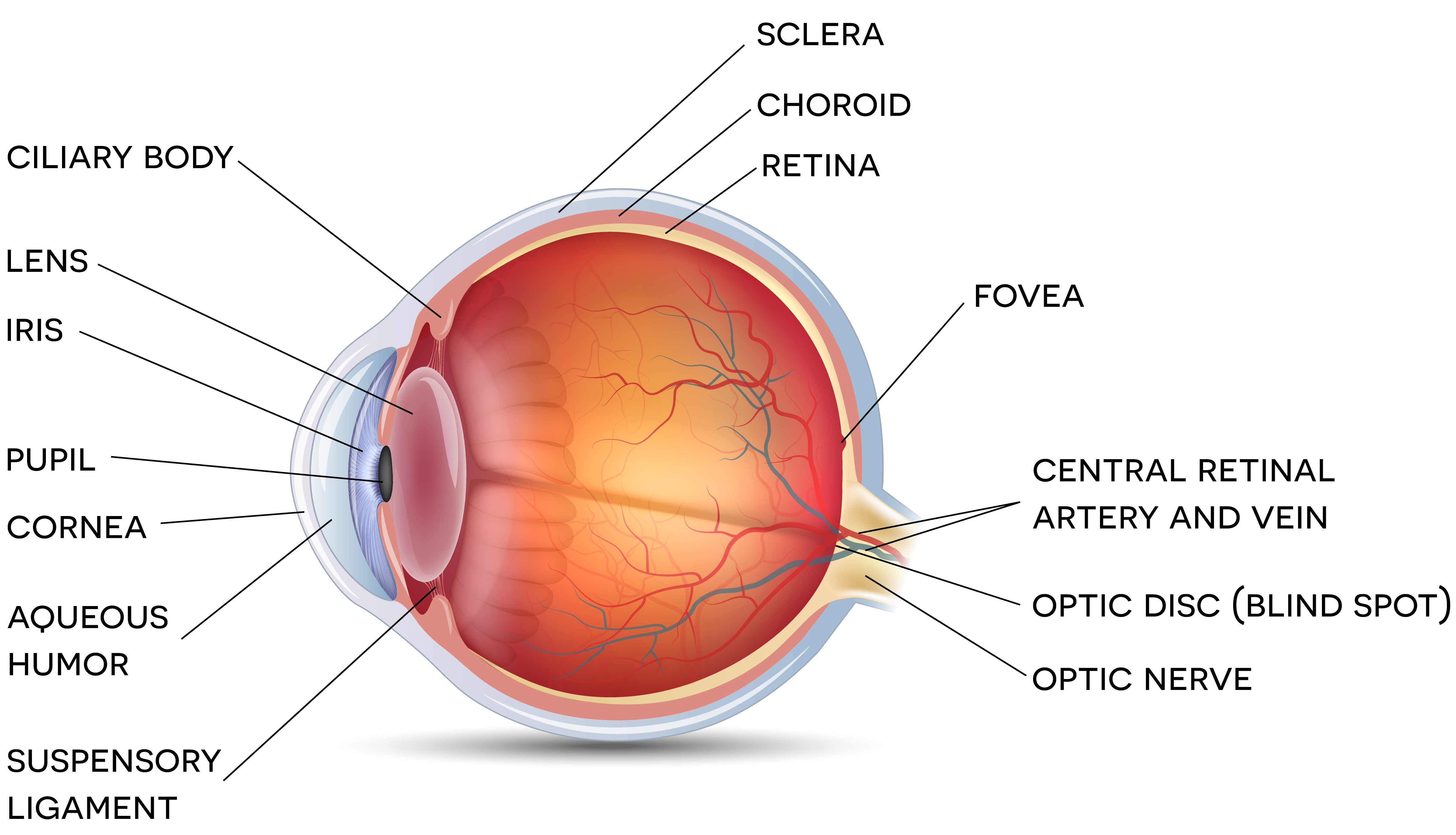
Fig. 3: Anatomy of the eye
In 2004 and 2006 the medical literature reported macular retinoschisis in non-shaking circumstances.[20] The shaken eye corollary to the shaken baby hypothesis is based on traction between the vitreous of the eye and the retina, or vitreoretinal traction, which is more pronounced in infants than adults. In 2002 the shaken eye corollary to the shaken baby hypothesis was characterized as “biomechanically improbable”[21] and by 2009, whether vitreoretinal traction played any role in causing retinal hemorrhage was characterized as “controversy”[22]. New case reports continue to surface clearly demonstrating that the eye findings Dr. Levin boldly declared in 2000 as “diagnostic” of shaking is simply not true.
Doubt, yet prosecutions continue unabated
Despite the controversy over shaking as a mechanism for subdural hemorrhage and retinal hemorrhage, and a complete retreat from the hypothesis that subdural hemorrhage was a marker for diffuse axonal injury, prosecutions of the caregiver present at the onset of symptoms in alleged shaken baby cases continues unabated. The proponents of the shaken baby hypothesis, have simply reformulated the hypothesis and its associated presumptions and follow a different triad. “Children who are otherwise healthy and have no history of trauma … who present with subdural hemorrhage and unexplained skeletal injuries, … or severe retinal hemorrhages generally are presumed by most physicians to have a non-accidental mechanism of injury.”[23] [24]
“Unexplained” Fractures
The new triad is subdural hemorrhage, retinal hemorrhage and “unexplained” fractures. Proponents of the shaken baby hypothesis advise, “[e]vidence of other injuries, such as bruises, rib fractures, long-bone fractures, and abdominal injuries, should be meticulously searched for and documented.” If the initial exam fails to reveal any evidence of trauma, proponents further urge “[r]epeated physical examinations may reveal additional signs of trauma.” In search of “unexplained” fractures, according to the American Academy of Pediatrics, a “skeletal survey of the hands, feet, long bones, skull, spine, and ribs should be obtained as soon as the infant’s medical condition permits” and “a skeletal survey should be repeated after 2 weeks to better delineate new fractures that may not be apparent until they begin to heal (a process that does not become radiologically apparent for 7–10 days).”
Fractures that are not fractures
The search for “additional signs of trauma” other than subdural or retinal hemorrhage, implies subdural and retinal hemorrhage are, by definition, traumatic. The search for “other signs of trauma” leads to some situations where fractures that do not exist are interpreted from the imaging and used to support a shaken baby diagnosis. It is not unusual for “possible” and “suspected” skull, rib, tibia, fibula, ulna and radius fractures to be interpreted from imaging when there are no such fractures. In cases where true fractures or pseudofractures[25] (bone findings that appear to be fractures but are not) are present, the presumption of abuse often prevents a genuine search for a metabolic cause of subdural hemorrhage or “unexplained” fractures.
Not proven medical or scientific fact
According to Dr. Norman Guthkelch, the pediatric neurosurgeon often credited with first advancing the hypotheses, the shaken baby syndrome hypothesis and its associated shaken eye hypothesis are “simply hypotheses, not proven medical or scientific facts” and that it is not reasonable to “infer shaking (or any other form of child abuse) from a finding of retino-dural hemorrhage of infancy”[26].
New terminology, same lack of evidence
The fact that the shaken baby syndrome hypothesis could not be confirmed in the laboratory didn’t stop medical doctors from promoting the hypothesis as if it were fact. When it became apparent that science didn’t support the SBS hypothesis, the medical doctors promoting it changed the terminology to shaken impact syndrome. Despite the change in terminology, the medical profession has never abandoned the notion that even when there is absolutely impact or trauma, a brain bleed can be caused by shaking alone. Because a growing minority of doctors has been challenging and dissenting from the shaken baby syndrome hypothesis, in 2009 the American Academy of Pediatrics recommended yet another change in terminology. Now the American Academy of Pediatrics recommends the term Abusive Head Trauma to avoid identification of a mechanism of injury. Whatever it is called, the hypothesis is flawed and creates a danger to innocent parents. In fact, the American Academy of Pediatrics has taken the position that the mere presence of a subdural hematoma alone, without any other evidence of abuse, gives rise to a presumption that the cause of the subdural hematoma is non-accidental or inflicted trauma unless the parents can provide an accidental explanation or “history”. This presumption based on a flawed hypothesis has almost universally been adopted by the child protective services community and law enforcement and has been the cause of many innocent parents, caregivers and boyfriends being arrested and/or having their children taken away.
Sources:
[12] Duhaime AC, Durham S (2007) Traumatic brain injury in infants: the phenomenon of subdural hemorrhage with hemispheric hypo- density (“big black brain”). Prog Brain Res 161:293–302
[13] Mack J, Squier W, Eastman JT (2009) “Anatomy and Development of the Menings: Implications for Subdural Collections and CSF Circulation.” Pediatr Radiolog. Mar 39(3) 200-210
[14] Case ME, Graham MA, Handy TC, Jentzen JM, Monteleone JA, for the National Association of Medical Examiners Ad Hoc Committee on Shaken Baby Syndrome. Position paper on fatal abusive head injuries in infants and young children. Am ] Forensic Med Pathol 2001 ;22: 112-122.
[15] Geddes J et al., Neuropathy of Inflicted Head Injury in Children: I. Pattern of Brain Damage, Brain 2001; 124(7):1290-1298. Geddes J et al., Neuropathy of Inflicted Head Injury in Children: II. Microscopic Brain Drain Injury in Infants, Brain 2001; 124(7):1299-1306.
[16] Dias MS. The Case for Shaking. In: Jenny C, editor. Child Abuse and Neglect. Elsevier Saunders; 2010.
[17] Wyngnanski-Jaffe T, Morad Y, Levin AV, Pathology of retinal hemorrhage in abusive head trauma, Forensic Sci Med Pathol (2009) 5:291–297 DOI 10.1007/s12024-009-9134-4
[18] In his writings, Dr. Alex Levin almost universally substitutes the word “macular” for “traumatic” essentially equating “macular retinoschisis” with “traumatic retinoschisis”.
[19] Levin A. Retinal haemorrhage and child abuse. In:David T, ed. Recent Advances in Paediatrics. London, England: Churchill Livingstone; 2000:151-219.
[20] Lantz PE, Sinal SH, Stanton CA, Weaver RG Jr. Perimacular retinal folds from childhood head trauma. BMJ. 2004;328(7442): 754 –756; Lueder GT, Turner JW, Paschall R: Perimacular retinal folds simulating nonaccidental injury in an infant. Arch Ophthalmol 2006; 124:1782-1783
[21] Ommaya AK, Goldsmith W, Thibault L. Biomechanics and neuropathology of adult and paediatric head injury. Br J Neu- rosurg. 2002;16(3):220–242
[22] Clarke, MP, Controversy: Vitreoretinal traction is a major factor in causing the haemorrhagic retinopathy of abusive head Injury? – No, Eye (2009) 23, 1761–1763; doi:10.1038/eye.2009.200; published online 7 August 2009Levin AV, Controversy: Vitreoretinal traction is a major factor in causing the haemorrhagic retinopathy of abusive head Injury? – Yes, Eye (2009) 23, 1758–1760; doi:10.1038/eye.2009.199; published online 7 August 2009
[23] Rorke-Adams L, Duhaime AC, Jenny C, Smith WL, Head Trauma; In: Child Abuse, Medical Diagnosis and Management, 3rd Edition; Christian CW, Reece RM, Editors(2009), American Academy of Pediatrics.
[24] “Shaken baby syndrome is characterized by the triad of skeletal injury, intracranial hemorrhage, retinal hemorrhage, or a combination thereof, usually in the absence of external signs of injury.” Schloff S, Mullaney PB, Armstrong DC, et al. Retinal findings in children with intracranial hemorrhage. Ophthalmology. 2002; 109:1472–6. See discussion below on the new triad.
[25] One type of fracture that proponents of the shaken baby hypothesis consider diagnostic of abuse is the Classic Metaphyseal Lesion (CML). CMLs are typically found in the growth plate of long bones and exhibit none of the healing phases characteristic of other bone fractures. There are some doctors who doubt CMLs are fractures at all and are, according to the doctor most credit with “discovering” CMLs, characterized as “resembling” and “indistinguishable” from rickets, “similar” to bone dysplasias, “simulate” and “difficult to distinguish from” from developmental bone variants. Kleinman PK, Problems in the diagnosis of metaphyseal fractures, Pediatr Radiol (2008) 38 (Suppl 3):S388–S394 DOI 10.1007/s00247-008-0845-6. In short, CMLs are likely “normal developmental variants and dysplastic changes that may be confused” and misdiagnosed as child abuse. Due to the epidemic of vitamin d insufficiency, it is thought that many CMLs are simply infantile rickets misdiagnosed as abusive fractures, particularly in infants under six months of age.
[26] Guthkelch, AN, Problems of infant retino-dural hemorrhage with minimal external injury; 12 Hous. J. Health L. & Policy 209 (Nov. 28, 2012).